Stewardship
Let's fight against AMR
What is Stewardship?
Stewardship can be defined as a careful and responsible management for the optimization of antimicrobial use. (1) It’s a healthcare system-wide approach to promote and monitor judicious use of antimicrobials, to preserve their future effectiveness (2), based on interventions designed for: (3)
- Measuring antibiotic prescribing (3)
- Improving antibiotic prescribing by clinicians and use by patients so that antibiotics are only prescribed and used when needed (3)
- Minimizing misdiagnosis or delayed diagnoses leading to underuse of antibiotics (3)
- Ensuring that the right drug, dose, and duration are selected when an antibiotic is needed (3)
«Antimicrobial stewardship is the optimal selection, dosage, and duration of antimicrobial treatment that results in the best clinical outcome for the treatment or prevention of infection, with minimal toxicity to the patient and minimal impact on subsequent resistance». (2)
Antimicrobial stewardship is one of the three pillars of an integrated approach to health systems strengthening, that includes infection prevention and control, medicine and patient safety. (1)
Linked to other key components, such as antimicrobial resistance surveillance and adequate supply of safe medicines, it promotes equitable and quality healthcare in order to achieve universal health coverage. (1)
Antimicrobial stewardship interventions can be performed in all types of healthcare facilities and should be aligned with local needs, addressing areas where observations or data suggest the need for improvement and where the outcomes of the implemented interventions are measurable. (1) It is extremely important that healthcare providers recognize the need and the value of stewardship plans and support them in healthcare facilities. (2)
According to the Organisation for Economic Cooperation and Development report (OECD), implementing antimicrobial stewardship programmes, along with other policies to reduce the overuse of antibiotics and promote hospital hygiene, could save up to 1.6 million lives by 2050 and $ 4.8 billion per year only in the 33 OECD countries. (1)
Developing best practices for the rational use of antibiotics is the main aim of an antimicrobial stewardship programme. This can be performed under different aspects, such as: (1)
- Optimizing the use of Antibiotics (1)
- Promoting behaviour change in prescribing and dispensing practices (1)
- Improving quality of care and patient outcomes (1)
- Saving unnecessary healthcare costs (1)
- Reducing further emergence, selection, spread and impact of antimicrobial resistance (1)
Antibiotic stewardship programmes
Antibiotic stewardship programmes can rely on fundamental core elements such as: (2)
- Leadership commitment, providing necessary human, financial and information technology resources (2)
- Accountability: appointing a single leader responsible for program outcomes. Experience with successful programs show that a physician leader is effective (2)
- Drug expertise, appointing a single pharmacist leader responsible for actions to improve antibiotic use (2)
- Action, implementing systemic evaluation of ongoing treatment needs after a set period of initial treatment, intravenous-to-oral programs, prospective audit and feedback, antibiotic restrictions (2)
- Tracking, as monitoring antibiotic prescribing and resistance patterns (2)
- Reporting, with regular updates on antibiotic use and resistance to doctors, nurses and relevant staff (2)
- Education, involving and updating clinicians about resistance and optimal prescribing (2)
How to implement an Antimicrobial Stewardship programme
A key outcome of antimicrobial stewardship interventions in healthcare facilities, is a change in behaviour in antibiotic prescribing practices over time, leading to more
responsible use. (1)
Experience shows that antimicrobial stewardship programmes can be successfully implemented when healthcare structures and procedures are available and in place. As a result, essential core elements have been identified to help countries build the necessary structures at the national (state/regional) level to enable health-care facility AMS programmes, considering the local context. (1)
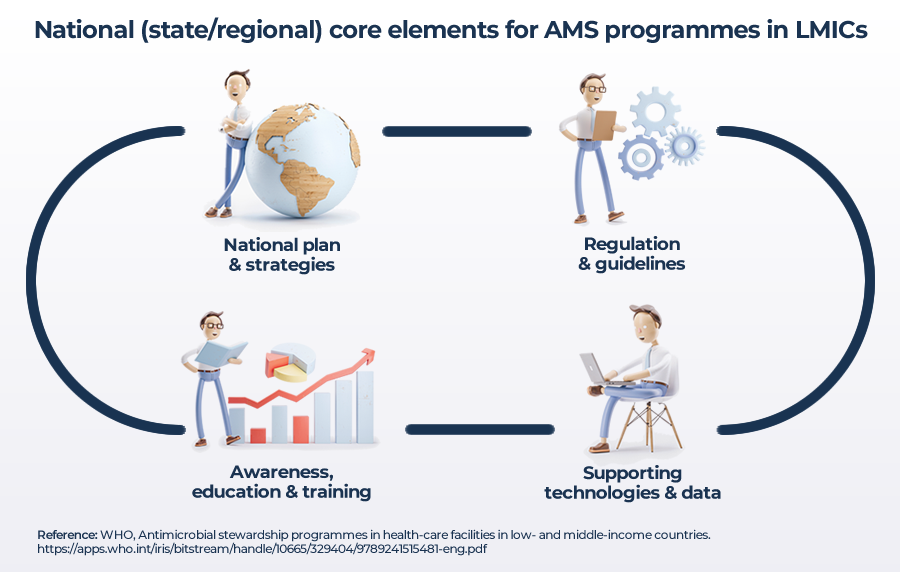
Source: ANTIMICROBIAL STEWARDSHIP PROGRAMMES IN HEALTH-CARE FACILITIES(1)
Antimicrobial stewardship interventions should be implemented in a stepwise approach, built on existing structures and reporting. They should also maximize teamwork and encourage personnel and clinical staff, including prescribers, to participate by starting from small, simple and long-lasting actions. (1)
The implementation process requires a tailored approach to address the different factors that may influence antibiotic prescribing and use in a specific context, such as: (1)
- Involving clinical staff in identifying local targets for improving antibiotic use (1)
- Having a systematic approach to implementing AMS interventions (1)
- Reviewing progress over time (1)
- Making changes when appropriate (1)
«Implementation research provides methods to promote the uptake of proven clinical treatments, practices, organizational and management interventions into routine actions to improve health». (1)
The implementation process also identifies the behaviour of healthcare professionals and organizations as key sources, before effective uptakes can be finally achieved. (1)
Therefore, implementing evidence-based antimicrobial stewardship interventions, to change prescribing behaviour, means taking into account factors that influence prescribing and using them to develop the facility action plan. (1)
Infection Prevention and Control (IPC) as an implementation tool
IPC is a practical and evidence-based approach which aims to prevent patients and healthcare workers from being colonized with bacteria or acquiring infections. This action not only prevents healthcare-associated infections and deaths, but it also saves money, reduces the spread of antimicrobial resistance and supports high-quality health services. (1)
Implementation of IPC programmes can be achieved by creating strong links to antimicrobial stewardship programmes and other initiatives addressing antimicrobial resistance, as well as enhancing patient safety and quality of care with a complementary approach which aims to prevent the spread of resistant bacteria and infections by reducing the overuse and misuse of antibiotics. (1)
As a result, collecting data on the use of antibiotics is also important to assess the extent and quality of antibiotic use. Identifying problematic prescribing practices and comparing them with appropriate use in healthcare facilities, is recognized as an implementation tool. (1)
Measuring the quantity and appropriateness of antibiotic prescribing and use can help improve the targeting and monitoring of antimicrobial stewardship interventions, even though each type of data collection, related to antibiotic consumption, use and audit, can have its own advantages and disadvantages. (1)
How does Stewardship help in the fight against Antimicrobial resistance?
With antimicrobial resistance rates increasing worldwide and few new antibiotics being developed, existing antibiotics are becoming a limited resource. It is therefore essential that antibiotics and last-resort antibiotics are reserved for patients who truly need them. (1)
«Optimizing the use of antibiotics is critical to effectively treat infections, protect patients from harms caused by unnecessary antibiotic use, and combat antibiotic resistance». (4)
Antibiotic stewardship programmes can help clinicians improve clinical outcomes and minimize harms by reducing: (4) (2)
- Treatment failure
- Adverse effects
- Length of treatment
- Antibiotic resistance
- Hospital costs and lengths of stay
- Morbidity and mortality
Antibiotic stewardship can be used in all healthcare settings in which antibiotics are prescribed. It remains a cornerstone of efforts aimed at improving antibiotic-related patient safety and slowing the spread of antibiotic resistance. (2)
The main goal of antibiotic stewardship programmes is to maximize the benefit of antibiotic treatment while minimizing harm both to individuals and to communities. (3)
MC-ID-01-2021
- WHO_Antimicrobial Stewardship Programmes
- BSAC_Antimicrobial Stewardship_From principle to practice
- CDC_Core Elements of Outpatient Antibiotic Stewardship
- CDC_Core Elements Of Hospital Antibiotic Stewardship Programmes